Welcome to The Auricle!
Read The Auricle’s first edition for 2024 (January-April) !
The Auricle is now live for 2024! Follow this link to find the new issue and this one to learn more about it!
In this issue, you’ll find an interview with Professor Rosemary Nixon for our Humans of Medicine panel. Dr Rosemary is a renowned dermatologist who has won membership of the Order of Australia (AM) for her contributions to Occupational Dermatology, and is the only person in Australia to have qualifications in both Dermatology and Occupational Medicine—and she is also a Monash Medicine Alumna!
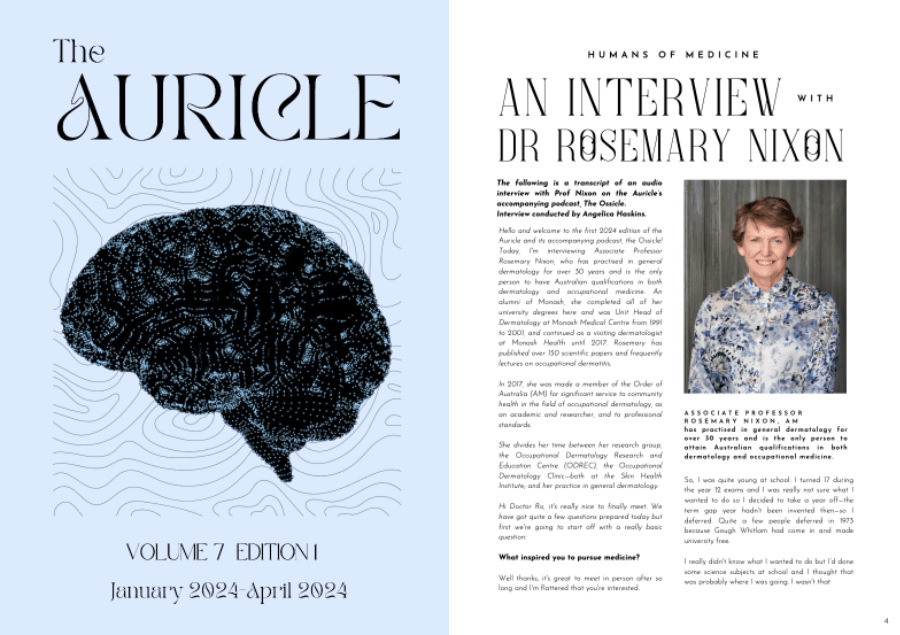
This issue also contains evocative creative and retrospective pieces from many talented members of our cohort. These pieces are often an outlet for our student body to express themselves through the medium of fiction, or to dissect deeper feelings about placements that have left long-lasting impressions.
Read The Auricle‘s final Edition for 2022: Edition 5 (October-December)!
We are thrilled to present to you our October-December Edition – follow this link to see the full magazine!
The Creative Writing and Visual Art Competition 2022 is over!
See here for the full list of winners.
Click this link to see all winning entries!
At The Auricle we are proud to showcase the talent of a wide variety of medical students at Monash University. See below a feature of some of our most popular posts from 2022.
The Auricle is back in 2022 with a new editorial direction – see here for more!